Note: this article quotes three of us from the ALS community — Andrea Lytle Peet, Larry Falivena, and me.
NC residents with severe health problems worry about COVID vaccine delays
BY HANNAH SMOOT
FEBRUARY 22, 2021 12:15 PM,
Charlotte Observer
https://www.charlotteobserver.com/news/coronavirus/article249317405.html?fbclid=IwAR25TUIuqccm7JzGdzYV7kcLnkIL2iQSkB4hIjIZFMNqbkSUDmMErqTcuT8
For Maura Wozniak’s family, wearing masks and social distancing is nothing new.
The Huntersville woman has cystic fibrosis, and has undergone two double lung transplants. She wears a mask every time she goes to the doctor’s office or hospital — even before the coronavirus pandemic hit — to protect herself and her lungs.
When vaccines first became available, the state prioritized certain groups of people to get the vaccine first — and people with chronic illnesses were initially in an early group. So Wozniak began making plans for after her vaccinations — including sending her kids back to school in person, for one.
Instead, the state changed priority orders. So Wozniak, like thousands of North Carolinians dealing with chronic or even terminal health conditions, must wait until three other groups get vaccines first. And that could take weeks or months.
The delay in getting vaccines has added to the worries of people like Raleigh resident Andrea Lytle Peet, who has ALS. “This time is really precious to us,” she said.
NC CHANGES VACCINE PRIORITIES
In an October plan, North Carolina first divided the vaccine rollout into phases that prioritized the order in which groups would be vaccinated. That plan, and the composition of the priority groups, has changed multiple times since then.
In the earliest plan, people with chronic health conditions were in Phases 1b and 2. Adults age 18 through 64 with one chronic condition — which the state estimated would include roughly 557,000 to 775,000 North Carolinians — fell into the same category (Phase 2) as essential frontline workers, like law enforcement and teachers.
But in late December, the state announced it had updated its vaccination plan — moving the frontline essential workers to Phase 1b. Adults with medical conditions that increased the risk of severe COVID-19 complications would fall under Group 2.
Top of Form
Bottom of Form
“The changes simplify the vaccine process and continue the state’s commitment to first protect health care workers caring for patients with COVID-19, people who are at the highest risk of being hospitalized or dying, and those at high risk of exposure to COVID-19,” the N.C. Department of Health and Human Services said at the time.
In mid-January, the vaccination plan was updated once more, moving away from the phased breakdown and separating North Carolinians into broader groups.
Now, people like Wozniak fall into Group 4, the last group prioritized before vaccine eligibility opens up to the general public. And frontline essential workers — which the state estimated could include up to 441,000 people — are prioritized in Group 3, ahead of people with chronic health conditions.
Wozniak said she has heard people argue that unlike essential workers, people with chronic conditions can just stay home. But that’s not true, Wozniak said.
Last and early winter, Wozniak said she was at the doctor’s office once or twice a week. And just this month, she had surgery at Atrium Health, staying in the hospital for two nights.
For people with chronic conditions, not going to doctor’s appointments isn’t an option, she said. “You’re putting yourself at risk by going in — and you have to go,” Wozniak said. “It’s essential.”
LOSING TIME
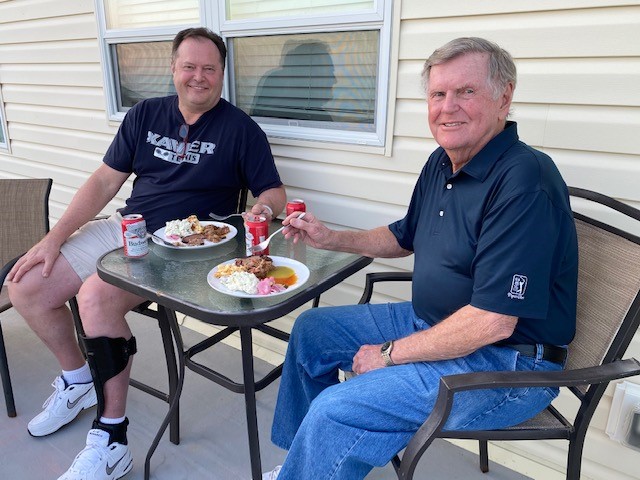
Apex resident Larry Falivena was diagnosed with ALS in 2017. ALS is a terminal disease. The average survival time is about three years, according to the ALS Association.
Progression of ALS can mean losing the ability to speak and breathe, which means catching a respiratory virus like the coronavirus could be deadly.
At the same time, staying home to avoid exposure to the coronavirus means losing time with loved ones or missing out on experiences people with terminal diseases may not be able to get back, Falivena said.
“You don’t know how much time you have left,” Falivena said.
“So you try to make the most of life. But then on the other hand, now there’s COVID, that puts you at greater risk,” he said. “It’s kind of this strange balancing act of. If I don’t do this now, will I be able to? But at the same time, it’s not worth the risk (of catching COVID-19).”
Like most people, Falivena’s family, including his 16-year-old and nearly 14-year-old sons, have canceled trips and vacations to limit the spread of COVID-19. But like Wozniak, Falivena can’t fully isolate. He’s in a clinical research study at Johns Hopkins, so he flies to Maryland once a month.
Every time he goes to Johns Hopkins, he’s most interested in the tests that evaluate his breathing capacity.
“Losing the ability to breathe is is the biggest factor in terms of longevity of life with ALS,” Falivena said. “…Now you’re facing a virus that attacks and damages your lungs and your nervous system. Maybe even permanently.
“Then to learn that now you’re near the bottom of the list for receiving that vaccine. It was pretty disheartening, especially for people who already need something to hope for.”
FEARING FOR FRIENDS DURING COVID
Lytle Peet, who turned 40 last week, was diagnosed with ALS when she was 33.
She has some trouble speaking due to ALS, but feels lucky that she’s been able to maintain her breathing for so long. Lytle Peet credits that to exercising. She swims every week, meeting her mom at the Life Time pool in Raleigh. They do water aerobics, keeping masks on even in the water.
And she’s done 25 marathons, using a recumbent bike. Lytle Peet is trying to be the first person with ALS to do a marathon in every state.
Her most recent marathon was in December. Fewer people than normal ran, due to COVID-19. But it was still “pretty nerve-wracking” to be in public during the pandemic, she said.
It was a shock to Lytle Peet when she realized people with chronic conditions wouldn’t be able to get the COVID-19 vaccine until after thousands of others took their turns.
“I think of my friends who are declining fast than I am,” she said. “To think that they are spending their last months isolated, away from loved ones, for fear of the virus — that weighs on me. Most people have decades ahead of them. But we don’t.”
‘A MATTER OF LIFE AND DEATH’
Many people with ALS in N.C., including Lytle Peet and Falivena, wrote to the NC COVID-19 Vaccine Advisory Committee. They asked it to press the state Department of Health and Human Services to reconsider the prioritization plan, that puts people with chronic health conditions in Group 3.
Davidson College Professor Ken Menkhaus, an ALS Association Board of Trustees member, said getting the COVID-19 vaccine is “a matter of life and death” for people with chronic health conditions.
The main difference between the state’s first vaccination plan and the current one is the shifting of people with chronic health conditions behind frontline essential workers, Menkhaus said.
“That’s a huge group of people,” Menkhaus said of essential workers. “You get behind that, and you’re months and months away from getting a vaccine.
“The message that they sent, whether they meant to or not, is that our lives matter less than other members of the community,” said Menkhaus, who was diagnosed with ALS in 2018.
North Carolina DHHS did not answer a question from The Observer about whether the state has plans to reassess the priority groups. But DHHS spokeswoman Catie Armstrong said in a statement: “The vaccine prioritization is designed to save lives and prevent spread while vaccine supplies are limited.”
The state is aligned with CDC recommendations on priority order, Armstrong said.
Wozniak understands the vaccine rollout can’t be perfect. Still, she says the state has had months to plan for this and put priority groups in place.
“For someone like me, who fought like hell to live through two double lung transplants, and am in the prime of my life with a young family — I don’t want to get this (virus),” she said. “I want the vaccine. I want to be able to go on.”